COVID-Related Coagulopathy, Take 3*
A Conversation with a Hematologist
By Ruth Werner
I’m a pathology educator for massage therapists, so ever since weird blood-clotting patterns started showing up in the news about COVID-19, I have been tracking this—maybe a little obsessively. And, as more information came out, my alarm grew. A couple of months later (could it be such a short time?) we have some more information—and enough understanding—to know that some of our “best guesses” so far have put us on the right track for client safety.
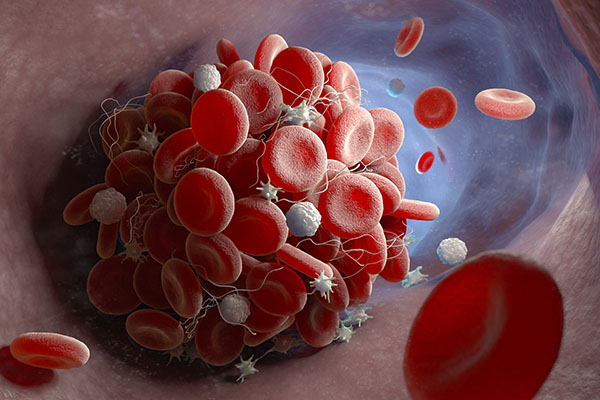
We know that abnormal coagulation is part of the pathologic picture with COVID-19. Autopsies of patients who died from this infection often show signs of systemic blood clotting, which contributed to multiple organ failure and death. This coagulopathy could be directly linked to the viral invasion of endothelial cells, but many other factors appear to contribute, including changes in the blood-clotting process, out-of-control inflammation, and more. Severe coagulopathy appears to be most common among hospitalized patients with the most serious cases. But what do we know about this risk for patients who have mild to moderate infections?
I was honored to have a conversation with Yaser Diab, MD, a hematologist working at Children’s National Hospital in Washington, DC. Right now, he spends most of his time with patients who have MIS-C (multisystem inflammatory syndrome in children), a result of COVID-19 in young patients. “It is the bane of our existence,” he said, although happily, the prognosis for his patients is generally very good.
Dr. Diab often sees massage used in hospitals, but he was less familiar with the practice of massage therapy in outpatient settings. I gave him an overview of what massage looks like for fundamentally healthy clients, and we talked about our profession’s special cautions regarding deep vein thrombosis (DVT) and pulmonary embolism risk. Then we discussed where massage therapy might fit in the context of COVID-19 survivors and coagulopathy. Here are some notes from our conversation:
• On the risk for coagulopathy in mild-to-moderate cases—several unknowns
Extreme, body-wide, uncontrolled coagulation is a cause of death for some COVID patients, but this situation is much rarer in mild to moderate cases. (This echoes my recent conversation with an immunologist as well.) That said, massage therapists are rightly concerned about unknown blood-clotting risks for their clients who may have otherwise recovered from COVID-19.
How common are low-level blood-clotting problems among people who are not hospitalized with COVID? We don’t know—but low-level problems are not associated with high risks of embolization. How long does the risk of coagulopathy remain after a person recovers from their infection? We don’t know. However, we do know that the signs and symptoms of thrombosis are the same in this population as for anyone else.
I described our current massage therapy screening processes: asking about new pain with exertion, especially chest pain or pressure; skin lesions; and activities of daily living, so that we get a clear idea of our clients’ cardiopulmonary function and general resilience. Dr. Diab suggested also checking for any signs of DVT as well, just to be on the safe side—these include subtle or obvious unilateral leg pain, discoloration, or swelling.
Dr. Diab asked about our protocols regarding anticoagulant therapy. I told him we can work with people who use anticoagulants or blood thinners, but we recommend lighter pressure to avoid the risk of bruising, and he felt this was appropriate. I asked how long anticoagulants might be prescribed for COVID patients, and learned that when these drugs are used as a preventive, it’s usually for 30 days or less, but when they are used as a treatment for someone who has already been identified with clotting problems, the prescription is typically for three months or more. So, if we have a client with an established history of coagulopathy, we can expect they will be on some kind of blood thinner or anticoagulant for at least three months.
• On why some people seem to get so much sicker than others
We know that the virus invades ACE-2 receptors, which are found on many cells throughout the body. It turns out that some people have many more ACE-2 receptors than others, and this may be a factor in how susceptible they are to the virus, and how severe their infection is.
Further, while some people seem to have mild infections with few, if any, long-term repercussions, others clearly have much more serious versions of the disease. It may be that the people with the most severe illness are those who have exaggerated inflammatory responses to the virus—this takes us back to the cytokine storm reactions that have been discussed elsewhere.
Dr. Diab suggested we may be able to find an identifiable predilection for this inflammatory overreaction, and eventually it may be possible to predict who is most at risk, and who therefore must take the greatest precautions against contracting the disease.
• On the deep muscle and joint pain that some people experience—what is happening, and is massage appropriate?
Many COVID patients and survivors report deep, severe, widespread muscle and joint pain. Dr. Diab confirmed there are three possible explanations: rhabdomyolysis (muscle degeneration that leads to kidney damage), poor tissue perfusion due to hypoxia, and microvascular thrombosis.
If it is rhabdomyolysis, the pain is likely to be both extreme and localized, and there would also likely be urinary symptoms. These are reasons for a client to cancel a massage, and go to the doctor instead. But if the pain is due to hypoxia or microvascular thrombosis, gentle massage is likely to be safe, and the pain relief we can offer may be very helpful.
• On the connections between microvascular clotting and embolization—and implications for massage therapy
The microvascular damage seen with COVID-19 and the risk of embolization from clots in larger vessels (leading to heart attack, stroke, and pulmonary embolism) may be part of the same process, or they may be two different entities—this is not fully known. However, the warning signs of potentially dangerous embolization for COVID patients are the same as they are for the general public. For this, we must refer back to signs and symptoms of DVT. If any of these are present, the client must be referred to emergency services.
However, if the client only has signs of microangiopathy (damaged small blood vessels) in the skin (e.g., COVID toe, petechiae, and other discolorations, bruises, or rashes), then the risk of a dangerous embolism is much lower. One new piece of information I learned is that histological examinations of COVID-toe lesions do not show thrombosis—capillaries are damaged, but blood clots are not present. This is an interesting finding, although it probably doesn’t change anything about our work.
The upshot, according to Dr. Diab, is that too much pressure on or close to skin lesions could contribute to bruising, but as long as the discoloration or rash is isolated and there are no other signs of DVT, then the risk of embolization (that is, inadvertently causing a pulmonary embolism) is not significant. Deep sigh of relief.
This is also consistent in what I’ve found in my conversations with patients with have had COVID-related skin lesions: many of them are physically very active, and they have no ill effects. Therefore, gentle massage is unlikely to cause any greater disruptions.
The Takeaways
I shared the strategies I have so far recommended for screening our clients who have come through COVID infections, and Dr. Diab confirmed that they are appropriate—with the addition of checking for DVT.
These recommendations include:
- Establish that the client is not communicable.
- Establish that the client does not have observable signs of DVT (e.g., unilateral redness, swelling, leg pain).
- Establish that the client does not have new (that is, since their infection) pain with exertion (e.g., shortness of breath, chest pain, dizziness, headache, cramping).
- Get a clear picture of the client’s activities of daily living.
- Work especially lightly over any skin lesions like rashes or petechiae (and of course avoid skin that is not intact).
- Work especially lightly if the client uses anticoagulants, either as a preventive or as treatment.
- Work gently to start, and check the next day to see how the massage was tolerated. Increase the intensity of massage gradually, over the course of several sessions.
My deepest gratitude to Dr. Diab, who took time away from his young patients to discuss this important information with me. This isn’t the be-all and end-all of post-COVID screening—new information arises all the time, and we must be willing to adapt on the fly. But it is so good to know we’ve been on the right track so far.
*Take 1: “COVID-19-Related Coagulopathy” by Ruth Werner
*Take 2: “Questions for Client Who Have Had COVID-19” by Ruth Werner
author bio
Ruth Werner is a former massage therapist, a writer, and an NCBTMB-approved provider of continuing education. She wrote A Massage Therapist’s Guide to Pathology (available at BooksofDiscovery.com) now in its seventh edition, which is used in massage schools worldwide.