Be sure to read the special COVID-19 digital-only issue of Massage & Bodywork magazine.
By Sasha Chaitow, PhD
See what I just did there? Can I ask readers to take a moment and consider what their internal reaction was to that headline? One of urgent curiosity to read on and find out “the truth,” or a flash of irritation at what looks like clickbait? Mixed feelings? Did anyone stop to check who’s writing this column or what the source is?
Whatever your response, you’d be right. In the course of an average day during lockdown, you’re bound to come across several dozen similar headlines—more often than not leading to speculative pieces on what might or might not be happening to our world with varying degrees of accuracy.
Let’s face it: this is possibly the single most impactful major event in our lifetimes, and it’s hard not to get caught up in a desperate search for information on the science behind the situation. As epidemiologists, infectious disease specialists, and all manner of experts take to the airwaves to advise, admonish, and inform us, a lot of contradictory information is flying around. Official-looking titles and well-crafted articles selling either hope or fear can suck us in quite easily, but after an hour or so of scrolling and clicking in the hope of making sense of it all, we can end up more confused than when we started.
To cut through the noise, it would make sense to go straight to the research itself. Following World Health Organization (WHO) policy put in place following lessons learned from the 2014–2016 Ebola outbreak, scientific publishers worldwide agreed to make all research and data on public health emergencies freely available, so that all scientists could access information and pool resources and efforts toward developing a vaccine and/or curative drugs.1 This has been applied to the current COVID-19 crisis. Reflecting the speed of virus spread, they also prioritized peer review and online pre-print publication to make every snippet of research available quickly, and research databases are now flooded with new studies daily.
The downside of the broad availability of so much new research is that while we have masses of it, there is very little quality control, and there has not been enough time for full peer review to be conducted. This caveat is included on most hubs hosting COVID-19 research. It is meant for other researchers who are scrambling to develop an understanding and potential cure for the virus, and it is generally assumed they will apply their expertise in their appraisal of each emerging study, in a kind of community-based peer review. That’s where research literacy is not just a useful skill; it becomes a critical part of the race for a vaccine and/or antiviral drug.
However, this material is almost indecipherable to the general public, and in general, science journalists have been playing fast and loose with it, adding to the overall confusion. In gathering material for this article, I was genuinely shocked to see the degree of misinterpretation applied to some of the COVID-19 research papers, with the story changing as it travels around the world. Even some of the data from the WHO contains errors and omissions, which a British group of scientists is now attempting to complete and correct.2
To be fair to science journalists and regular reporters, they too are struggling to make sense of this sudden information overload. Yet, the golden rule of science journalism that should apply to anyone who is conversant with—but not expert in—the specifics of virology, epidemiology, and infectious diseases, is: don’t be afraid to admit what you don’t know, check your sources, and ask an actual expert. The second golden rule is: remember that science is messy. So messy, that even the experts are openly uncertain as to the true data surrounding this pandemic. It is natural to want clear answers in such frightening times, but it is also important to understand the limitations of science and to avoid spreading misinformation.
The Big Questions
The questions being asked by the experts are very similar to those being asked by journalists and the public:
- Am I in danger?
- Who has this disease? (And who dies from it?)
- How can I stay safe?
- Where did it come from and why?
- Is there a cure? (And why is it taking so long to find?)
There are many conflicting answers flooding the airwaves, but not because of how they are expressed. The answers are contradictory because of the context and the worldview of who is asking—and answering—the question.3 A medical specialist understands the fine details of pathophysiology (the processes that occur to make people sick); a layperson does not have that training. Although we are throwing around phrases such as cytokine storm, inflammatory process, or monoclonal antibody because they are being reported in the news, even physicians in unrelated specializations may not be fully equipped to understand their inner workings. This is one of the reasons why public-facing information is generally simplified into a set of instructions, without too much medical detail. These are often frustratingly perfunctory—and do not answer our many questions—but if they come from a source such as the Centers for Disease Control and Prevention (CDC) or the WHO, we can be reasonably confident that they are based on the most recent science and are reliable. News media sources and their snappy infographics cannot necessarily be trusted even if they use the right jargon, because even science journalists can misinterpret information.
Why Smart People Believe Junk Science
Right now, everybody’s judgment is a little compromised, and with good reason. When we seem to be looking at a story full of contradictions that threatens us directly and disrupts our way of living, the mind tries to make sense of what is happening by developing perceptual hypotheses to fill in those gaps. Educated guesswork and a form of patternicity—“the tendency to find patterns in meaningless noise”—takes hold.4 Depending on the sociocultural, educational, and psychological makeup of the individual, different forms of apophenia may be experienced, which is the tendency to ascribe intention, meaning, and connections between seemingly random data and events, and is often the basis for conspiracy theories.
In short, if a story isn’t making sense to us, we fill in those gaps with what we do know and understand. Scientists are not immune to this; what is known as type 1 error in statistics is the tendency to see false patterns in data or incorrectly ascribing causality. Researchers and data analysts are just as likely to fall prey to the phenomenon as the layperson, but the stakes are higher since the information they extract from reams of data may be used at the highest levels to develop policy and governance.
Evolutionary modeling has shown that patternicity is an ancient survival mechanism, based on the relative risk of potential outcomes depending on which pattern is believed. Not looking for patterns (and creating them where we can’t find them) creates intolerable anxiety because of the degree of uncertainty, and therefore the potential perceived danger. For example, believing that the noise in my apartment corridor is a burglar when it is only my cat will prompt me to investigate. If I believe it is my cat and do nothing, I might be murdered in my bed. But if I believe it is a burglar and act on that, I have a fighting chance of survival, so thinking the worst “costs” me less than ignoring the noise. Compounded with other psychological and experiential factors, researchers in evolutionary biology have concluded that, in general, modern humans are not good at judging the relative probability of one scenario over another, and if we cannot understand the causes behind something, we will tend to “assign causal probabilities to all sets of events . . . lump[ing] causal associations with non-causal ones.”5
Faced with a worldwide pandemic that has created this degree of disruption compounded by tons of data we are struggling to make sense of, our brains fall into the pattern of meaning-making and ascribing causality, with the added stimuli of fear and anxiety. The survival threat is real, and we have few tools at our disposal. We are being told to act in ways that feel unnatural, to self-isolate and abandon our jobs, our families, everything that forms our routine and identity.
As we try to gain control over the situation, we search incessantly to satisfy burning questions even though we may not have the tools to interpret what we’re looking at when we do find the research. Enforced isolation makes things worse; there is a sense of urgency, a need to communicate and share, to feel we are contributing in some way, to protect our own. On a grand scale, with the help of social media and instant communication, misinformation becomes widely held belief. If we are not conscious of our own thought and communication patterns, then instead of contributing to our survival, we are actually contributing to the problem.
In such a climate, another key misconception can get in the way, which I touched on in a previous column (“A Cautionary Tale,” March/April 2020, page 46, www.massageandbodyworkdigital.com/i/1208028-march-april-2020/48). This is the idea that science is all-powerful and that expert opinion—or what the media presents as expert opinion—is absolute. Surely if we go directly to the research, so readily available, we will understand more, be correctly informed, and be safer. Unfortunately, this is not the case: expertise is not the same as infallibility, and while scientists have knowledge and powerful tools at their disposal, there is also much that they do not know; as noted earlier, statistics are also prone to error.
Communication Noise
Any chain of communication, at its most basic, looks like the illustration below.
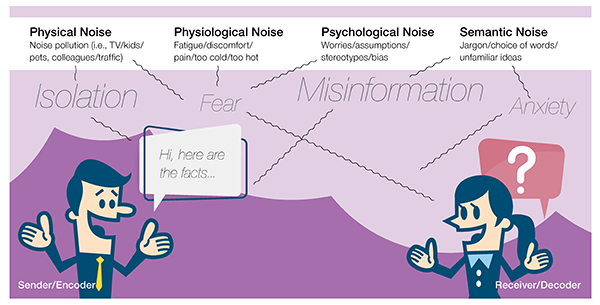
Add a threat to survival, and the noise increases and the likelihood of accuracy decreases. Particularly when dealing with a threat involving disease and public health, those in positions of authority often stumble when attempting to communicate public health policy and complex medical information to the general public. Essentially, the scientific community has one narrative, based exclusively on the data; the layperson has another; and the educated adjunct to the health professions is somewhere in between.
Each of these groups will develop their own narratives that subconsciously reflect their own understanding of the situation, with their own anxieties and fears built in. Just as is the case when examining patient values and preferences in a therapeutic scenario, public health and political officials need to address these anxieties and narratives if they are to be heeded. Not doing so often leads to widespread panic and noncompliance on the part of the wider public because they simply do not believe what the authorities are saying.
People may prefer to believe rumors and anecdotes because they still have a human, emotional dimension, which is stripped away in scientific, factual language, leading to clear miscommunication between the scientific and lay communities.6 Narratives that fill in the gaps provide meaning, make the situation relatable, and satisfy the anxiety caused by the situation. In a public health emergency, these factors fall by the wayside as officials rush to face the more immediate threats of contagion and mortality. If scientists and science-literate officials and practitioners can cater to these needs, then it may be possible to improve the overall response to situations such as COVID-19.
What We Can Do
The best we can do is attempt to reduce the layers of “noise” by looking at the evidence, while bearing in mind at all times that this, too, may be subject to error. However, rather than allowing our subconscious fears and prejudices to fill in the gaps of what we do not understand, we can still have some control over the conclusions we reach. It is then up to us to find ways of communicating this with our unique psychosocial context in mind.
Calling out and shaming people for considering unscientific narratives has no place in this: people are frightened, just as individual patients may be afraid or crippled with anxiety due to a given condition. Even if we are not infected with COVID-19, the contagion of fear is almost as dangerous. Bodyworkers have highly developed skills when it comes to exercising and expressing compassion, and those skills are crucial. If we can identify where we, too, are allowing contagious narratives to cloud our judgment and educate ourselves first and foremost, we can then transmit that understanding to others in the same way we would speak to a client in acute pain. This is every bit as important as the work being done in labs to find a vaccine for COVID-19.
Here is a list of some key misconceptions and beliefs seen in headlines and online discussions in recent weeks. It is by no means exhaustive, but I have chosen some of the more common or outlandish claims seen in headlines and shared by members of the bodywork community in recent days and weeks. For each, I have sourced the most recent, relevant research, and critically appraised whether they stand up to scrutiny. To do so, I have asked the following questions:
- What is the source?
- Who are the authors? What are their qualifications and conflicts of interest?
- Is this peer-reviewed article?
- How old is the source?
- Are there additional sources confirming or disagreeing with my source? If so, what seems to be the consensus view?
- What do the major independent institutions (CDC, WHO) say regarding the information in my source?
- What, if any, discrepancies do I see in the source with an untrained eye?
If the source material falls at any of these hurdles, and the discrepancies cannot be explained away as a failure on our part to understand the material because it is too technically complex, then it would be wise to refrain from fully believing it, and more so, refrain from sharing it unless it is with a colleague whose scientific understanding is more sophisticated.
True or False?
COVID-19 is no more dangerous than the flu
This misconception has been partially responsible for the slow responses of some governments around the world to address COVID-19. The actual answer is complex and uncertain. This uncertainty is due to a lack of scientific data on the virus, which specialists are having to study in different real-world environments as the pandemic evolves, rather than from the safety of a controlled lab.
COVID-19 is a novel virus, meaning it has not been seen in humans before. The human immune system has not been exposed to it, and is therefore more susceptible to it. We do not yet fully understand all the risk factors. It is much more contagious than influenza, partly because of the lack of immunity, and partly because of the longer asymptomatic incubation period. Understanding the role of time in relation to the life cycle of a virus is key to understanding how and why it spreads.7
It is thought that over time, more people will develop immunity to the virus, and with the help of a vaccine, it will be possible to reduce the risk it poses to levels similar to those of common flu. However, we simply do not yet have enough information to judge this. According to the current understanding, COVID-19 causes a severe type of pneumonia in enough individuals to make the mortality rate around six to 10 times higher than that of the common seasonal flu.8 It may be possible, in months and years to come, to reduce this rate or to access data that changes our understanding of the true mortality rate. However, as explained in a study looking at the mortality rate in Wuhan, China, any current estimates are based on uncertainties and what is known as “ascertainment bias,” which is when a population sample does not fairly represent the target population (in this case, the total number of people affected).9
As different countries are taking vastly different approaches to testing, we do not currently know the true number of infected people (cases) and therefore cannot accurately calculate the true fatality ratio. This ongoing report from CMMID Repository (caution advised: it is not yet peer reviewed) provides some interesting concerns regarding the reporting methods and mathematical models used to estimate the numbers we all hear in news reports, and demonstrates the degree of uncertainty currently surrounding the issue.10
What we know beyond any doubt is that whatever the true case-fatality ratio (number of people who die out of all those infected), more people need critical care simultaneously than our health systems can handle, and that in and of itself will lead to more deaths. This is the true source of the crisis regardless of whether or not it turns out to be more or less lethal than influenza once the current crisis has died down.
Note About Source Reliability
Take a quick look at the Johns Hopkins source cited at the end of this article. You might notice that it states the date 2017. Many uninformed readers could jump to the conclusion that I have used an outdated source, or that COVID-19 has been around for longer and the current hysteria is all a hoax. That kind of thinking is how conspiracy theories are born, and they put people in danger. The actual reason for this is because the Johns Hopkins ABX guides were originally developed in 2017. At the time of writing, this guide states: “Updated: March 23, 2020.” This is what is meant by “due diligence” when appraising any source. Two excellent nonspecialist sources to refer to if the raw research is too complex are The Conversation, written by academics for the non-specialist layperson; and the Johns Hopkins Hub. Both provide further information on recent research and key issues surrounding the current pandemic.11
Research Letters Are Not the Same as Research
Due to the urgency of the situation, researchers are collecting as much data as they can, as fast as possible, under strained circumstances. They are not observing the stringent statistical methods used in more carefully designed clinical trials or observational studies because the current situation does not allow for that. The articles themselves describe the methods undertaken, which were clearly chosen to attempt to provide raw data to the scientific community. This is valuable information, but comes with the caveat that it has not yet undergone full scientific screening.
True or False?
Only old people die of COVID-19, so young and healthy people don’t need to worry
This is the second major misconception that has contributed to the rapid spread of this virus, leading to difficult conversations that weigh economic factors against the cost of human life. The truth is we don’t yet know precisely who is at most risk, beyond obviously vulnerable elders with multiple underlying conditions.
Since COVID-19 reached Europe and the US, there have been reports of younger, healthy people dying and skewing the numbers somewhat, and these figures are also affected by the degree of testing being conducted. Recent demographical information from the Johns Hopkins Information Center suggests early data from the US sees more young adults hospitalized (20–44 age range; 20 percent of hospitalizations; 12 percent of intensive care unit [ICU] admissions). Germany is another outlier with a median patient age of 47 years, and a very low death rate (0.4 percent, lower than that of the common flu).12 Germany has taken a different approach to testing and hospitalization compared to other countries, reflecting its advanced health-care infrastructure, which plays an important part in the overall outcome.
When it comes to public health policy, the overall capabilities of any health service and its accessibility and capacity are key factors in calculating the virulence or mortality rate of a given pathogen. Overcrowding, a lack of ICU capacity, and overstretched medical staff drive up the mortality rate just as much as the effects of the virus itself. It may yet be that more people die because of late—or no—access to health care, and this is something that is still undecided. Given the reality in different countries around the world, this is an area that will need considerable reexamination once the current crisis is over.
For the time being, it is clear that common sense must be adhered to; elderly people and all those with chronic conditions are more vulnerable to pathogens in general.
True or False?
We just need to boost our immune systems by taking lots of vitamin C and other supplements, and/or use essential oils/crystals/herbal remedies and our body will fight off the virus
This may be an opportunity to debunk one of the most widespread misconceptions about our health: it is not possible to “boost” the immune system in the sense of guzzling oranges and vitamin supplements or using external applications of oils or anything else to increase the number of microscopic “soldiers” in our bloodstream in an otherwise healthy human. Hot water, hairdryers, and mammoth doses of vitamins are not going to kill the virus either.13
Before that gets misinterpreted, let me be clear: it is certainly possible to weaken our body’s responses to pathogens through bad habits, poor diet, high stress, or immunosuppression caused by certain lifesaving treatments (corticosteroids, chemotherapy, etc.). And an overactive immune system is not something anyone wants. An overactive immune system leads to autoimmune conditions such as rheumatoid arthritis and so on, though it is not possible to simply “cause” these by taking supplements.
The good news is that someone in good health, whose lab tests are all in the “normal” zone, and who generally eats, sleeps, exercises, and avoids bad habits (such as smoking) simply needs to carry on as they are. It is neither necessary nor possible to “bank” immune defenses by swallowing additional vitamin C, for example, because the body cannot store the vitamin, so it simply keeps what it needs and disposes of the rest (possibly causing an upset tummy in the process). Attempts to use vitamin C intravenously can be deadly and are currently limited to experimental or carefully controlled uses. The same goes for herbal remedies that may support organ function or detoxification, but can be lethal in high quantities. Essential oils, herbs, and other such materials may do a lot to help us de-stress, and used appropriately, they can add to our overall well-being and help us counter anxiety at this difficult time. But none of these remedies can kill a virus. In up to 80 percent of infected people, their immune system may indeed be able to do that on its own if they experience a mild expression of COVID-19, but some patients will need additional treatment and support.14
In addition, reports on what happens in critical cases of COVID-19 suggest that one of the most dangerous phases is what is known as a “cytokine storm.” This is when our own immune system overreacts to the invading virus and overcompensates by producing extreme inflammation that stops the lungs from being able to continue with normal gaseous exchange that occurs with normal breathing. This is where ventilators and drugs are needed to reduce inflammation by immunosuppression (stopping the immune overreaction) and to ensure that oxygen reaches the bloodstream through the lungs. Reports currently suggest that the timing of each stage of this treatment may be critically important to reducing the worst effects of COVID-19-induced pneumonia, and front-line physicians are still attempting to reach a consensus on those steps.15
Unfortunately, quick-fix ways to fight the virus using homemade remedies are very popular online, with the vast majority being utter fantasy. This is another one of those cases where attempting to regain control over our lives can easily lead to buying into, or actively sharing, misinformation and possibly doing more harm than good.
True or False?
COVID-19 can be transmitted through all bodily fluids so we should not donate blood
This was a recent query I received, which demonstrated the degree of conflicting information currently available. One example from a reliable source that demonstrates the degree of confusion comes from the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota.16 The source cites a number of articles published in reputable scientific journals, which conclude that it remains unclear whether the virus is transmitted via aerosolization (dispersal through the air). These conclusions derive from two research letters published in the Journal of the American Medical Association (JAMA) and Emerging Infectious Diseases respectively.17
For example, the JAMA article states that samples of body secretions (various respiratory specimens from the nose, mouth, and lungs, as well as feces, blood, and urine) were taken from patients at different times during their illness, and these are compared against basic demographic and pathological data, though not all clinical information was available, and not all secretions were collected from all patients. One percent of patients did have positive viral test results in their blood, but there is no information on what their stage of disease was, or any other clinical data. The authors clearly state that this is not enough information to form clear conclusions, but that further, more systematic research is necessary. The CIDRAP source summarizes the article information accurately.
However, this is the kind of information that a less sophisticated reader may seize on as “evidence” for transmission via blood, and through an oversimplified, carelessly worded article, begin to spread misinformation. This is precisely the kind of example where great care is needed to understand the relative value of the source—and why we must choose our words with care.
According to the Johns Hopkins source cited earlier, and based on what now seems to be majority consensus formed as physicians and researchers gain more experience of this virus, transmission occurs by respiratory droplets and fomites (objects on which droplets may have fallen). This information is confirmed by the American Red Cross, citing the US Food and Drug Administration (FDA) and the CDC.18 According to current knowledge, the virus does not spread through blood, but even if it does, screening is in place to ensure that infected blood does not reach blood banks.
True or False?
Some blood types are immune or less susceptible to COVID-19 than others
This misconception recently made the rounds on news media around the world, and is based on an article found on medRxiv, the preprint server for health sciences.19 The abstract inspires hope at first glance: a retrospective study comparing blood group distribution among 2,173 confirmed COVID-19 patients from three Chinese hospitals at the heart of the outbreak, with healthy people in the same regions. The paper concludes that: “People with blood group A have a significantly higher risk for acquiring COVID-19 compared with non-A blood groups, whereas blood group O has a significantly lower risk for the infection compared with non-O blood groups.” It further notes that neither age nor gender appear to have any effect on the distribution.
This article reads like breakthrough information until we take a closer look at some details. First, this is a pre-print release. It has not been peer reviewed or evaluated, as stated in the disclaimer at the top of the page. This should be a red flag for any reader.
Second, if we examine the data presented by the authors in relation to the claims made in the conclusion of the paper, there seems to be a discrepancy between the numbers and the claims made. There are certain minor language issues that may be responsible for some unclear points, but the concluding statement is unequivocal, even though there are several gaps in the research and reporting.
To begin with, we are not told the normal distribution of blood types across the general population of that region. Type O blood is the most common worldwide, therefore the authors’ conclusion that Type A blood is overrepresented in the COVID-19 sample appears to be correct.20 However, it is an easy point to overlook, giving rise to suggestions that the authors have misinterpreted the results—they do not seem to have, but it is expressed poorly. Secondly, no information is given regarding comorbidities (other illnesses), treatment choices, or exposure for the infected population, and there has been no consideration regarding the effect this may or may not have had on their exposure to infection and need for hospitalization. The sample of people used in the study were all in the “severe” or “critical” disease category (or deceased), therefore it is unclear whether Type A blood groups were more susceptible to infection, or to severe disease.
The omission of all these elements can lead to overwhelming bias within a study, making the results far less reliable than the report initially suggests. Further, surprisingly, rhesus blood type was not included in the study, which could have revealed significant data. And lastly, the use of the word significantly higher or lower, while commonly used to discuss scientific statistics, is easy for lay readers to misinterpret as “important.” In scientific terminology, significance refers to whether something can statistically be assigned to chance or not. It is an either/or binary category and not an indication of degree of importance. However, to judge by the pingbacks and links listed below the article since its publication on March 16, it appears that few science journalists have taken this into account.
In short, though the article may provide findings of value to virology researchers and the interaction of pathogens and antiviral medication, it is the kind of material where great caution is needed.
True or False?
There is a conspiracy to remove civil liberties and COVID-19 is the excuse
This is not a scientific issue, and some may query why I have listed it here. Conspiracy deserves a column of its own, as it is perhaps one of the most common opinions currently circulating, expressed in various forms by healthy skeptics and conspiracy theorists alike. It is important in this context, firstly because those who still doubt the reality of COVID-19 may also be those more resistant to following official guidance on physical distancing and quarantining, leading to additional infections. Secondly, questions are being raised across society as to the practicability and ethics of long-term quarantining, as well as whether it will actually make a difference.
The answer to conspiracy theorists lies in economic and political reality: it is in nobody’s interest to crash worldwide economies and break social cohesion in this way. Secondly, global communication is not just freely available. It is enhanced at present, and at least in the Western world, there is no censoring of information. True conspiracies can only work under total secrecy; yet it is quite easy to confirm the veracity of the anguished reports coming from Italy, Spain, and elsewhere, and it is impossible to fabricate the amount of medical data being checked and double-checked before being undersigned by the WHO, CDC, and other major institutions. The rules of probability alone make it impossible to put all the moving parts of this unfolding crisis down to a global conspiracy. History teaches us that this kind of pressure in fact reveals hidden fault lines and social dramas within society; that is a far more interesting—and sobering—line of inquiry, since human judgment error in crisis management right now is a far more realistic and dangerous scenario than any secret elites plotting global domination.21
That civil liberties have currently been curtailed wherever full lockdown has been instituted is true, but in all locations these rules have also been given expiry dates, with legislative and governing bodies obliged to review and reconsider them every few weeks as the situation evolves. It is also true that if this crisis lasts for more than a few weeks, the economic, social, and labor situations may be permanently changed, but that does not equate with a permanent restriction of freedoms.
On the contrary, history has demonstrated that our temporary loss of civil liberties is likely to provide opportunities for growth, innovation, and perhaps, a unique chance to correct some of the most problematic systems in developed countries, including those that have impacted the environment. This is an area worth exploring, particularly if your business has been impacted by the current lockdown, and the links below provide commentaries and food for thought for those interested in exploring the question further.22 An excellent source exploring related issues is the “SNF Agora Conversations,” available through the Johns Hopkins hub, where experts from a variety of fields discuss and debate the political and policy implications of the handling of the COVID-19 crisis.23
True or False?
We have the cure!
Chloroquine has made international headlines, spurred on by recent US presidential statements. Numerous other drugs have been mentioned in international news sources as potential “cures” for COVID-19, with various governments ordering them by the truckload in the hope of lowering the mortality rate.
Both the research and WHO guidelines reveal a rather different picture than the news reports. At the time of this writing, there is no proven effective intervention for COVID-19. The medication cocktails being used are off-label and highly experimental, with wildly different approaches taken to disease staging (deciding when is the right time to apply certain types of treatment) and treatment approaches (choice of drugs, use of ventilators, etc.).24 Some limited success has been seen in small trials and desperate cases. It is those small trials that have led to the current focus on chloroquine or its safer derivative, hydroxychloroquine, an anti-malarial drug, following reports of French trials based on Chinese in vitro (laboratory) studies.25
The most recent commentary also notes that optimal safe dosage has not yet been established, that the drug can be highly toxic if misused, and makes it clear that more research is needed before we know for certain whether these, and other drugs have a replicable effect, and what the safe timing and dosage is. An early French nonrandomized trial on the use of chloroquine and hydroxychloroquine to treat COVID-19 featured a very small number of subjects (n=20) with mild to moderate symptoms. While cautiously positive, this study will need to be repeated with a much higher number of subjects, including severe cases (and this raises ethical concerns).26 These are just some of the hindrances to finding appropriate treatments.
Other drugs tested in more robustly designed clinical trials do not yet seem to have generated positive results. A recent Chinese trial of the HIV protease inhibitors lopinavir/ritonavir combination yielded no sign of benefits.27 Two randomized controlled trials on Remdesivir—originally produced to treat Ebola—are available only in Chinese. Strong claims are being made in news reports stating there is clear evidence in favor of a Japanese antiviral drug called Favipiravir.28 However, digging deeper, the current “evidence” consists of claims made by the pharmaceutical company producing the drug, a pre-print that has not yet been peer-reviewed; a small-scale, nonrandomized study published in an engineering journal based at the Chinese Academy of Engineering; and a summary of all medications used and recommended by the National Health Commission in China during the peak of the outbreak. While illuminating, this document clearly outlines a process of trial and error, conceding that full trials have not been conducted regarding the safety and efficacy of these drugs, and concluding that far more detailed research is necessary before any of these can be considered as a standard and effective treatment.29 Finally, a recent review document listed all known trials currently under way and at various phases as of March 12, 2020.30 It is worth remembering that all reputable clinical trials should bear database registration numbers and follow the most stringent international reporting guidelines if they are to be considered reliable.31
Currently, there is no evidence available from full-scale controlled trials to clarify whether any of these medications or their combinations are safe and effective, as most of them so far have failed to stand up to robust testing. There have been several reports of people self-medicating and taking fatal overdoses of chloroquine since these trials were first reported on, in an extreme example of why so much care is needed with science reporting, and with interpreting the quality and content of what is presented as evidence.32

True or False?
COVID-19 antibodies are the cure!
This is one of the oldest methods used over a century ago to slow down outbreaks and epidemics. Decades ago, the blood of patients who had successfully convalesced from a disease (such as measles) was used, sometimes as crudely as by direct transfusion, to provide antibodies to those who had not yet caught it, in a form of primitive vaccination known as “convalescent plasma” or convalescent sera. More modern techniques would involve isolating the serum or plasma alone—a simple, easy, and safe technique.
A clinical trial is about to commence at Johns Hopkins to clarify the safety and effectiveness of using this method for COVID-19, and if results are promising, it may be recommended as a stop-gap method to provide a form of immunity on a grand scale until a proper vaccine can be developed. It is more effective when used for prevention, rather than in those already infected, and there are some known risks attached, which will be explored in the trials.
Transfusion is not equivalent to, or a replacement for, a vaccine. Using plasma is a crude approach because with this method, the biotechnicians do not isolate the COVID-19-specific antibodies, but provide the patient with the full range of antibodies in the donor’s plasma. This has two effects; it may water down the overall immune response, or it may confuse it. In addition, antibodies do not remain in the bloodstream permanently, but it may work as a temporary way to delay more infections and to protect frontline health-care workers until a vaccine emerges. Vaccines are altogether more sophisticated because they target specific aspects of the viral reproductive process and anatomy to stop it before it begins infecting host cells. However, the steps and time needed to produce a safe, effective vaccination may reach well into 2021, and despite the lengthy processes also needed to gain evidence and approval for the plasma method, it may be quicker and more effective if all the moving parts are able to coordinate.33
True or False?
COVID-19 is a bioweapon/experimental virus that (somehow) escaped from a laboratory
It’s not just conspiracy theorists asking this question; even scientists have not shied away from it. “The Proximal Origin of SARS-CoV-2” published on March 17, 2020, in Nature Medicine provides the latest roundup of what is currently known.34 This is a complex, copiously referenced, and carefully put together article that concludes: “Our analyses clearly show that SARS-CoV-2 is not a laboratory construct or a purposefully manipulated virus.”
The authors make a strong case, and cite earlier studies warning of the potential for zoonotic viruses (originating in animals and jumping to humans) that provide further evidence for the way that coronaviruses have the potential to lead to outbreaks among humans.35 Both the 2020 article and its 2015 predecessor updated in March 2020 (see note 35) pass the checks I listed earlier in the article, and sharp-eyed readers noticing that both are listed in Nature Medicine as “correspondence” rather than feature articles may be reassured that letters are fully peer-reviewed by the journal’s reviewers and editors, forming a clear-cut category within that journal’s editorial policy.36
In short, not only is there no evidence to support the claim that COVID-19 is a manufactured virus, there appears to be evidence that in fact proves it is definitely natural. The sources provided go into some detail to explain and cross-check the possibilities and there seems to be no reason to believe otherwise.
What Next?
As shown in the examples above, it is very easy to jump to conclusions, make assumptions based more on our own fears than on reality, and to make connections for which there is simply no evidence. Ideally, you should not take my word for this.
Compare the sources against the checklist provided earlier, and use your own judgment—but attempt to avoid reading more or less into the material than is present. It is crucial to realize that precisely because this virus is new, there are still many unknowns. “No evidence” or “incomplete evidence” is not the same as “negative evidence.” Unknowns are areas that need research and clarification—fewer words, not more.
At the beginning, I explained why it is almost impossible for human nature to accept holes in such life-changing narratives, but this may well be a valuable lesson for many communities, particularly those with healing as a vocation. The best we can do to shape those narratives into something that helps, rather than hindering the efforts being made by physicians, researchers, and the general public, is focus on developing rational coping mechanisms. It can help to understand how “noise” and subconscious patternicity hinder us from doing so, and the links in the Notes below provide many places to start.
By developing rational responses, understanding the need to link these to localized narratives so that they can be better understood, finding ways to explain them to others, and strengthening our own resilience, we ensure our survival, both physical and mental. This may be the most valuable tool for healing when the time comes to emerge from self-isolation and return to healing our communities.
With 20 years in teaching and over a decade in journalism and academic publishing, Sasha Chaitow, PhD, served as managing editor of the Journal of Bodywork and Movement Therapies from 2018–2020. Based between the UK and Greece, she teaches research literacy and writing for the sciences at the University of Patras, Greece. She is a professional artist, gallerist, and educator who exhibits and teaches internationally.This article also appeared in the special COVID-19 issue of Massage & Bodywork.
Notes
1. World Health Organization, “Policy Statement on Data Sharing by the World Health Organization in the Context of Public Health Emergencies,” World Health Organization Procedures, April 2016, https://www.who.int/ihr/procedures/SPG_data_sharing.pdf.
2. Max Roser, Hannah Ritchie, and Esteban Ortiz-Ospina, “Coronavirus Disease (COVID-19)—Statistics and Research,” 2020, www.ourworldindata.org/coronavirus.
3. Jon D. Lee, An Epidemic of Rumors: How Stories Shape our Perceptions of Disease (Boulder: Utah State University Press, 2014), 2–3.
4. Michael Shermer, “Patternicity: Finding Meaningful Patterns in Meaningless Noise,” Scientific American 299, no. 6 (Dec 2008): 48, https://doi.org/10.1038/scientificamerican1208-48.
5. Kevin R. Foster and Hanna Kokko, “The Evolution of Superstitious and Superstition-Like Behavior,” Proceedings of the Royal Society B 276, no. 1654 (September 2008): 31–37, https://doi.org/10.1098/rspb.2008.0981; Sophie Fyfe et al., “Apophenia, Theory of Mind, and Schizotypy: Perceiving Meaning and Intentionality in Randomness,” Cortex 44, no. 10 (November–December 2008): 1316–25, https://doi.org/10.1016/j.cortex.2007.07.009.
6. Andrea Kitta, The Kiss of Death: Contagion, Contamination, and Folklore (Louisville, CO: Utah State University Press, 2019), 5–7.
7. World Health Organization, Coronavirus Disease 2019 (COVID-19) Situation Report—46 (Geneva: WHO, 2020), www.who.int/docs/default-source/coronaviruse/situation-reports/20200306….
8. Paul G. Auwaerter, “Coronavirus COVID-19 (SARS-CoV-2),” in Johns Hopkins ABX Guide, The Johns Hopkins University (March 2020), www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540747/all/C….
9. Kenji Mizumoto and Gerardo Chowell, “Estimating Risk of Death from 2019 Novel Coronavirus Disease, China, January–February 2020,” Emerging Infectious Diseases 26, no. 6 (June 2020), preprint accessed March 22, 2020, https://doi.org/10.3201/eid2606.200233.
10. Timothy W. Russell et al., “Using a Delay-Adjusted Case-Fatality Ratio to Estimate Under-Reporting,” CMMID Repository, March 2020, https://cmmid.github.io/topics/covid19/severity/global_cfr_estimates.ht….
11. Joseph Eisenberg, “RO: How Scientists Quantify the Intensity of an Outbreak Like Coronavirus and Predict the Pandemic’s Spread,” The Conversation, March 2020, www.theconversation.com/r0-how-scientists-quantify-the-intensity-of-an-….
12. Robert Koch Institute, “Coronavirus Disease 2019: Daily Situation Report of the Robert Koch Institute,” March 2020, www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte….
13. Arthur C. Macedo, Andre O. V. de Faria, and Pietro Ghezzi, “Boosting the Immune System, From Science to Myth: Analysis of the Infosphere with Google,” Frontiers in Medicine, July 2019, https://doi.org/10.3389/fmed.2019.00165; Beverly Merz, “What Can You Do to Improve Your Immune System?,” Harvard Health Publishing, September 2016, www.health.harvard.edu/healthy-eating/what-can-you-do-to-improve-your-i…; National Institute of Allergy and Infectious Diseases, “Overview of the Immune System,” Immune System Research, December 2013, www.niaid.nih.gov/research/immune-system-overview.
14. Paul G. Auwaerter, “Coronavirus COVID-19 (SARS-CoV-2),” in Johns Hopkins ABX Guide.
15. Irani Thevarajan et al., “Breadth of Concomitant Immune Responses Prior to Patient Recovery: A Case Report of Non-Severe COVID-19,” Nature Medicine, March 2020, https://doi.org/10.1038/s41591-020-0819-2; Puja Mehta et al., “COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression,” The Lancet 395, no. 10229 (March 2020): 1033–34, https://doi.org/10.1016/S0140-6736(20)30628-0. Note that both sources are in the form of peer-reviewed correspondence reflecting the ongoing developments and uncertainty within the medical community.
16. Mary Van Beusekom, “Study: COVID-19 May Spread in Several Different Ways,” CIDRAP News, March 2020, www.cidrap.umn.edu/news-perspective/2020/03/study-covid-19-may-spread-s….
17. Wenling Wang et al., “Detection of SARS-CoV-2 in Different Types of Clinical Specimens,” JAMA, March 2020, https://doi.org/10.1001/jama.2020.3786; Neeltje van Doremalen et al., “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS CoV-1,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMc2004973.
18. American National Red Cross, “What to Know about the Coronavirus and Blood Donation,” 2020, www.redcrossblood.org/donate-blood/dlp/coronavirus--covid-19--and-blood….
19. Jian Zhao et al., “Relationship Between the ABO Blood Group and the COVID-19 Susceptibility,” MedRxiv, preprint accessed March 2020, https://doi.org/10.1101/2020.03.11.20031096.
20. Worldwide ABO Distribution is: O+: 38.67%; A+: 27.42%; B+ 22.02%; AB+: 5.88%, with the remainder made up of the -Rh blood types. In China there are several different ethnic groups (Canton, Ningbo, Yangzhou, Peking, Han) with considerable variance between the distributions; for example among the “Peking” ethnic group, B is more common than O or A. This is due to genetic variance. Therefore, ethnic group information for this sample is actually quite important. Laura Clark, “World Population by Percentage of Blood Types,” WorldAtlas, July 2019, www.worldatlas.com/articles/what-are-the-different-blood-types.html.
21. David S. Jones, “History in a Crisis—Lessons for Covid-19,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMp2004361; Wendy E. Parmet and Michael S. Sinha, “Covid-19—The Law and Limits of Quarantine,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMp2004211; Lawrence O. Gostin and James G. Hodge Jr., “US Emergency Legal Responses to Novel Coronavirus: Balancing Public Health and Civil Liberties,” JAMA 323, no. 12 (February 2020): 1131–32, https://doi.org/10.1001/jama.2020.2025.
22. Eric Martin and Bloomberg, “Coronavirus Economic Impact ‘Will be Severe,’ at Least as Bad as Great Depression, says IMF,” Fortune, March 2020, www.fortune.com/2020/03/23/coronavirus-economic-impact-predictions-grea…; Lora Jones, David Brown, and Daniele Palumbo, “Coronavirus: A Visual Guide to the Economic Impact,” BBC News, March 2020, www.bbc.com/news/business-51706225; Politico Magazine staff, “Coronavirus Will Change the World Permanently. Here’s How,” Politico, March 2020, www.politico.com/news/magazine/2020/03/19/coronavirus-effect-economy-li…; Johann Fortwengel, “Coronavirus: Three Ways the Crisis May Permanently Change Our Lives,” The Conversation, March 2020, www.theconversation.com/coronavirus-three-ways-the-crisis-may-permanent….
23. Katie Pearce, “SNF Agora Institute Discussion Series Explores Policies, Politics of the Pandemic,” Johns Hopkins Hub, March 2020, https://hub.jhu.edu/2020/03/24/agora-coronavirus-series.
24. Hassan K. Siddiqi and Mandeep R. Mehra, “COVID-19 Illness in Native and Immunosuppressed States: A Clinical-Therapeutic Staging Proposal,” The Journal of Heart and Lung Transplantation, preprint accessed March 2020, https://doi.org/10.1016/j.healun.2020.03.012; Lisa Rosenbaum, “Facing Covid-19 in Italy—Ethics, Logistics, and Therapeutics on the Epidemic’s Front Line,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMp2005492; Robert D. Truog, Christine Mitchell, and George Q. Daley, “The Toughest Triage—Allocating Ventilators in a Pandemic,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMp2005689; Ezekiel J. Emanuel et al., “Fair Allocation of Scarce Medical Resources in the Time of Covid-19,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMsb2005114.
25. Jia Liu et al., “Hydroxychloroquine, a Less Toxic Derivative of Chloroquine is Effective in Inhibiting SARS-CoV-2 Infection In Vitro,” Cell Discovery 6, no. 16 (March 2020), https://doi.org/10.1038/s41421-020-0156-0.
26. Phillippe Colson et al., “Chloroquine and Hydroxychloroquine as Available Weapons to Fight COVID-19,” International Journal of Antimicrobial Agents, preprint accessed March 2020, https://doi.org/10.1016/j.ijantimicag.2020.105932; Phillippe Gautret et al., “Hydroxychloroquine and Azithromycin as a Treatment of COVIDâ€19: Results of an Openâ€Label Nonâ€Randomized Clinical Trial,” International Journal of Antimicrobial Agents, preprint accessed March 2020, https://doi.org/10.1016/j.ijantimicag.2020.105949; Chen Jun et al., “A Pilot Study of Hydroxychloroquine in Treatment of Patients with Common Coronavirus Disease-19 (COVID-19),” Journal of Zhejiang University, 49, no. 1 (March 2020), https://doi.org/10.3785/j.issn.1008-9292.2020.03.03.
27. Bin Cao et al., “A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19,” The New England Journal of Medicine, March 2020, https://doi.org/10.1056/NEJMoa2001282.
28. Jeanna Bryner, “Flu Drug Used in Japan Shows Promise in Treating COVID-19,” Livescience, www.livescience.com/flu-drug-could-treat-coronavirus.html.
29. Chang Chen et al., “Favipiravir Versus Arbidol for COVID-19: A Randomised Clinical Trial, MedRxiv, preprint accessed March 2020, https://doi.org/10.1101/2020.03.17.20037432; Qingxian Cai et al., “Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study,” Engineering, preprint accessed March 2020, https://doi.org/10.1016/j.eng.2020.03.007; Liying Dong, Sasha Hu, and Jianjun Go, “Discovering Drugs to Treat Coronavirus Disease 2019 (COVID-19),” Drug Discoveries and Therapeutics 14, no. 1(March 2020): 58–60, https://doi.org/10.5582/ddt.2020.01012.
30. Sandro G. Viveiros Rosa and Wilson C. Santos, “Clinical Trials on Drug Repositioning For COVID-19 Treatment,” Pan American Journal of Public Health 2020, no. 44 (March 2020): e40, https://doi.org/10.26633/RPSP.2020.40.
31. International Committee of Medical Journal Editors, “Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals,” ICMJE, December 2019, www.icmje.org/icmje-recommendations.pdf.
32. Alonso Soto, “Nigeria Has Chloroquine Poisonings After Trump Praised Drug,” Bloomberg, March 2020, www.bloomberg.com/news/articles/2020-03-21/nigeria-reports-chloroquine-…; ABC News, “Valley Man Dies, Wife Hospitalized after Taking Chemicals to Protect Them from Coronavirus,” ABC News, March 23, 2020, www.abc15.com/news/state/valley-man-dies-wife-hospitalized-after-taking….
33. Adam Rogers, “Blood From COVID-19 Survivors May Point the Way to a Cure,” Wired, March 24, 2020; Arturo Casadevall and Liise-anne Pirofski, “The Convalescent Sera Option for Containing COVID-19,” The Journal of Clinical Investigation, March 2020, https://doi.org/10.1172/JCI138003.
34. Kristian G. Andersen et al., “The Proximal Origin of SARS-CoV-2,” Nature Medicine, March 2020, https://doi.org/10.1038/s41591-020-0820-9.
35. Vineet D Menachery et al., “A SARS-Like Cluster of Circulating Bat Coronaviruses Shows Potential for Human Emergence,” Nature Medicine 2015, no. 21 (March 2020): 1508–13, https://doi.org/10.1038/nm.3985.
36. Springer Nature Limited, “Content Types,” Nature (2020), www.nature.com/nm/about/content.