Listen for an exploration of an extraordinarily complex autoimmune disorder with elements of lupus, scleroderma, and muscle inflammation. Includes short tangents on the etymology of the term pathognomonic and CREST syndrome (no, not the toothpaste.) Can massage help? Or is it off the table?
Resources:
Drugs.com. “Dermatomyositis.” Accessed June 3, 2021. www.drugs.com/cg/dermatomyositis-discharge-care.html.
Myositis Support & Understanding. “Scleroderma.” Accessed June 3, 2021. https://understandingmyositis.org/myositis-overlaps/scleroderma.
National Organization for Rare Disorders. “Dermatomyositis.” Accessed June 3, 2021. https://rarediseases.org/rare-diseases/dermatomyositis.
Ricceri, Federica and Francesca Prignano. “Gottron Papules: A Pathognomonic Sign of Dermatomyositis.” Canadian Medical Association Journal 185, no. 2 (2013): 148. https://doi.org/10.1503/cmaj.111791.
Schwartz, Noa et al. “Lymphatic Function in Autoimmune Diseases.” Frontiers in Immunology 10 (March 20, 2019). https://doi.org/10.3389/fimmu.2019.00519.
The Myositis Association. “Diagnostic Criteria for Dermatomyositis.” Accessed June 4, 2021. www.myositis.org/about-myositis/diagnosis/diagnostic-criteria/diagnostic-criteria-for-dermatomyositis.
VisualDx. “Dermatomyositis.” Accessed June 3, 2021. www.visualdx.com/visualdx/diagnosis/dermatomyositis?diagnosisId=51420&moduleId=101.

Gottron’s papules
https://commons.wikimedia.org/wiki/File:Dermatomyositis2.jpg


This podcast sponsored by:
About Anatomy Trains:
Anatomy Trains is a global leader in online anatomy education and also provides in-classroom certification programs forstructuralintegration in the US, Canada, Australia, Europe, Japan, and China, as well as fresh-tissue cadaverdissectionlabs and weekend courses. The work of Anatomy Trains originated with founder Tom Myers, who mapped the human body into 13 myofascial meridians in his original book, currently in itsfourthedition and translated into 12 languages. The principles of Anatomy Trains are used by osteopaths,physicaltherapists,bodyworkers,massagetherapists,personaltrainers,yoga,Pilates,Gyrotonics,and other body-minded manual therapists and movement professionals. Anatomy Trains inspires these practitioners to work with holistic anatomy in treating system-wide patterns to provide improved client outcomes in terms of structure and function.
Website:anatomytrains.com
Email:info@anatomytrains.com
Facebook:facebook.com/AnatomyTrains
Instagram: instagram.com/anatomytrainsofficial
0:00:00.0 Speaker 1: Ruth Werner's best-selling book, A Massage Therapist's Guide to Pathology is a highly regarded comprehensive resource that sets the standard for pathology education. Written for massage therapy students and practitioners, this ground-breaking resource serves up a comprehensive review of the pathophysiology signs, symptoms, and treatment of more than 500 diseases and disorders. Learn more at booksofdiscovery.com.
0:00:32.0 Speaker 2: Anatomy Trains is happy to announce our return to the dissection lab in person, January 10th to the 14th, 2022 at the Laboratory of Anatomical Enlightenment in Boulder, Colorado. We are thrilled to be back in the lab with Anatomy Trains' author Tom Myers, and master dissector, Todd Garcia. Join students from around the world and from all types of manual, movement, and fitness professions to explore the real human form, not the images you get from books. This is an exclusive invitation, email info@anatomytrains.com, if you'd like to join us in the lab.
[music]
0:01:16.8 Ruth Werner: Hi, and welcome to I Have A Client Who, pathology conversations with Ruth Werner. The podcast where I will discuss your real life stories about clients with conditions that are perplexing or confusing. I'm Ruth Werner, author of A Massage Therapist's Guide to Pathology, and I have spent decades studying, writing about and teaching about where massage therapy intersects with diseases and conditions that might limit our client's health.
0:01:46.1 RW: We almost always have something good to offer even with our most challenged clients, but we need to figure out a way to do that safely, effectively and within our scope of practice, and sometimes as we have all learned, that is harder than it looks. Today's story comes from a massage therapist in Nevada who shares this. I have a friend/client who is 56, she was diagnosed with dermatomyositis when she was 12. It's an autoimmune disease affecting the muscles and the skin, many steroids at the time. She has very restricted fascia and had Bell's Palsy and is diabetic. When I do some myofascial release, she has slight relief. I don't have the opportunity to work with her on a consistent basis, because we don't live in the same state. She receives acupuncture weekly now, which she says helps. She had surgery on the tendons of her hands, but she didn't do any physical therapy afterwards. I encouraged her to, but she said she was too busy. Unfortunately, she now realises this was a mistake. Is there any protocol or suggestions for therapy that you could offer? She's losing her ability to smile and the movement in her hands.
0:03:00.3 RW: Wow, okay. Let's pretend we have never heard of dermatomyositis, that name gives us some information, inflammation of the skin and muscles. Our contributor tells us it is autoimmune, and the person is experiencing some stiffening in her hands and her face. To me, this sounds a lot like scleroderma, an autoimmune condition that causes the skin in various places, especially the hands and the face to become thick and hard and unyielding. Hmm, let's find out some more. Emedicine.medscape.com, one of my favorite resources for high level information about diseases and conditions, tells us that dermatomyositis is an idiopathic inflammatory myopathy with characteristic cutaneous findings that occurs in children and adults. The systemic disorder most frequently affects the skin and muscles, but it may also affect the joints, the esophagus, the lungs, and less commonly the heart.
0:04:04.2 RW: So far, this sounds a lot like scleroderma, but as we learn more, the muscular component looks really different. People with dermatomyositis have skin issues for sure, but the way this disease affects skeletal muscles is different from what we see in most other autoimmune disorders. Dermatomyositis, I'll call it DM here as well, because it's easier to say, is pretty rare, rare enough to be listed in the National Organization for Rare Diseases at the National Institutes of Health. We think it affects about 10 people in every million. It is usually diagnosed in two groups, kids between the ages of 5 and 10, and adults over 50. Women get it about twice as often as men, which is typical for autoimmune diseases, and symptoms seem to come and go with no identified reasons. In traditional dermatomyositis, agents of the immune system, especially antibodies and abnormal T-cells launch an attack on the lining of small blood vessels and capillaries in the skeletal muscles of the extremities.
0:05:12.2 RW: The autoimmune activity leads to micro infarcts and the loss of muscle tissue, and because the supplying vessels are also damaged, the blood supply that would support local healing is blocked, so the muscles atrophy along with the fascia and scar tissue may develop. This autoimmune activity might be triggered by exposure to certain pathogens, but it has also been seen as a reaction to some drugs, and it often seems to run in family, so there's a genetic component as part of the picture as well. This all usually starts at the proximal limbs, lots of patients report that it's hard to climb stairs, hard to get up from sitting down or to reach for things, overhead, muscles in the head and neck can be weak too, so lifting one's head off the pillow can be really challenging. And the muscles that control the tongue and swallowing are sometimes affected, so speaking and eating are impaired.
0:06:06.5 RW: But about 40% of patients develop skin changes first long before any muscle symptoms are felt, and some people only have skin problems without any discernible muscle issues. This could be called amyopathic dermatomyositis. When skin symptoms are present, they resemble yet another autoimmune disease, lupus, with a unique kind of butterfly rash that stretches over the forehead, the eyes, the bridge of the nose and the cheek bones. A similar rash can develop in other areas too, especially the neck, chest and arms. The rash can be itchy, which interferes with sleep and it's made much worse with any exposure to sunlight. The facial rash is sometimes called a heliotrope rash, because on light-skinned people, it is a bright reddish purple color. In dark-skinned people, the discoloration is still present, but it may be subtler.
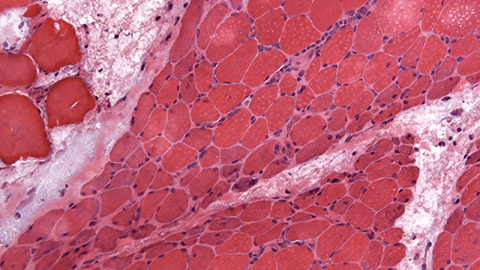
0:07:02.5 RW: When this heliotrope rash fades, sometimes it is followed by permanent discoloration, either darkening or lightening of the skin with atrophy and scarring. The hands of people with dermatomyositis can develop another characteristic sign, reddish-purple papules on the knuckles and the joints, these are called Gottron papules. The finger nails may show some changes with bluish red flakiness around the cuticles at the base of the nails and visibly dilated capillaries, these are sometimes called telangiectases. When these skin signs are seen along with the purple rash, they are so specifically associated with dermatomyositis that they are considered pathognomonic, that means belonging to or inseparable from a disease. This word comes from pathos, disease, and gnomon, one who knows. Sorry, I couldn't resist. I just love me some etymology.
0:08:03.0 RW: I'll put a photograph from Wikimedia in the show notes to show these Gottron papules and the characteristic changes in the cuticles. For some patients, the skin signs associated with dermatomyositis don't respond well to treatment, which is steroidal anti-inflammatories and protection from sunlight. And in severe cases, the skin on the hands may become thick and tight and the blood vessels may change, and this means it becomes increasingly difficult to use the hands and Raynaud's phenomenon could develop where blood vessels suddenly constrict and dilate, and this can be extreme and painful. The diagnostic criteria for dermatomyositis are sometimes divided into skin issues, musculoskeletal issues and others, not all of them have to be present all of the time. So in the skin, we expect to see that heliotrope rash on the face, dilated capillaries at the nail beds, Gottron papules, redness and itching over the shoulders and in front of the neck, sometimes this is also on the outside of the hip, and a skin biopsy will show changes in how the capillaries work.
0:09:10.3 RW: The muscular aspect of dermatomyositis includes these issues, progressive proximal symmetrical weakness, so the neck, shoulders, and upper arms and hips and thigh muscles get weak, elevated levels of muscle enzymes, especially creatine kinase, muscle and joint pain, an abnormal finding on electromyography, and this also helps to distinguish dermatomyositis from some other muscle weakening diseases like, amyotrophic lateral sclerosis, that's Lou Gehrig's disease, and myasthenia gravis, which is a different autoimmune issue. And muscle biopsies show that muscle fibers can become necrotic along with some other unique patterns. People with dermatomyositis may also have myositis specific antibodies and signs of systemic inflammation, like fever and inflammatory markers in the blood. The specialist who developed these criteria also suggests that DM has some subsets, including polymyositis, myositis with malignancy, and this is because adults diagnosed with dermatomyositis seem to have a way higher risk for certain kinds of cancers, and so, when it's diagnosed in adults that watch for those kinds of cancers begins.
0:10:23.7 RW: Childhood dermatomyositis or childhood polymyositis and myositis that overlaps with another collagen vascular disorder, and we'll get back to that in a moment. The relationship between skin problems and muscle problems in DM seems to be a little unpredictable. Sometimes the skin signs come up first, sometimes they follow the development of muscle problems by months or years. Sometimes skin issues are the only major symptoms and any muscle changes are so subtle, they only show up on tests, but they don't seem to impair function. And sometimes those muscle signs can change over time, so a person can experience weakness for a while and then it goes away. So the people who have led the way in documenting and treating dermatomyositis have noticed that it frequently overlaps with other collagen vascular disorders.
0:11:15.5 RW: We already saw the overlap between DM and certain aspects of lupus, especially in the facial rash and sensitivity to sunlight. There's enough overlap between DM and scleroderma that this combination has a name, scleromyositis. Other autoimmune diseases have overlapped too, but this triad of scleroderma, lupus, and dermatomyositis is particularly interesting. All three of these disorders involve autoimmune attacks that affect collagen in the skin and small blood vessels. And all three of them share a symptomatic phenomenon called CREST syndrome. This stands for calcinosis cutis, the development of hard nodules in the skin, and we see this mostly in children with DM. The R is for Raynaud's phenomenon, which we've mentioned. E is for esophageal dysmotility, this turned up in our initial description of DM, and it means that some people have a hard time with muscle function in the upper GI tract.
0:12:13.4 RW: S stands for sclerodactyly, which is what happens when the skin on the fingers becomes really hard and tight. And T stands for telangiectases, that refers to those small dilated capillaries that we see around the nail beds of people who have DM. Treatment for dermatomyositis, as well as for other autoimmune diseases, usually starts with high dose prescriptions of prednisone to reduce inflammation and suppress immune system activity. Of course, this is fraught with possible side effect, so it is not a long-term solution. But once the inflammation is under control, other interventions can include other kinds of gentler steroids, other immune system suppressants and lots of other drugs, in case those first line options don't work. And of course, lots and lots of sunscreen to protect the skin. And this is really good news because dermatomyositis is often highly treatable and we have lots of strategies to help with that.
0:13:14.3 RW: Well, that's a lot of complex information. What does it mean for our client in today's story? To review, she was diagnosed with DM at age 12, now at age 56, she has restricted fascia, she has a history of Bell's Palsy, which might not be connected at all. I'd sure love to do a podcast on Bell's Palsy, so please send me one of your stories. And she also has diabetes. She had some surgery on the tendons of her hands, it's not clear to me whether this was connected to her dermatomyositis or some other issue, but now she finds that her range of motion is limited. She receives acupuncture and she says it helps, and her friend also provided some myofascial release and that seemed to help too. Let's put all of this through our thinking machine and consider what are the possible risks and benefits for massage therapy for someone who has dermatomyositis?
0:14:10.4 RW: Here are some possibilities. If the client is in flare and has systemic inflammation with pain and fever and swelling, then careless or rigorous massage therapy could be overwhelming. Also, if she has to use high doses of steroids for a long period of time, this will have an effect on her tissues. Steroids can weaken connective tissue and fascia, and it may also have been a factor in her diabetes. Are there ways we can work safely? Sure, but let's delay anything with a deep physical impact until my flare has subsided, and then when she's feeling up to it, which is frankly, probably most of the time, because treatment is usually pretty effective for DM, well, we can add our work to improve the quality of her connective tissues, if that's your goal or to help with muscle and joint pain or to improve mobility and range of motion.
0:15:00.3 RW: I read a nice paper that I will put in the show notes that suggests lymphatic work might be helpful for people who have dermatomyositis, as well. Massage is probably not going to reverse the constrictive effects of DM, but we might be able to offer some temporary relief so that a client can move more freely and might be able to exercise more easily. People with dermatomyositis are encouraged to use warm baths and gentle exercise and massage to help with their symptoms. So, we can enthusiastically step up to be a careful, cautious and well-informed part of that disease management team.
0:15:41.8 RW: Hey everybody, thanks for listening to I Have A Client Who, pathology conversations with Ruth Werner. Remember, you can send me your I Have A Client Who stories to, ihaveaclientwho@abmp.com. That's ihaveaclientwho, all one word, all lower case, @abmp.com. I can't wait to see what you send me, and I'll see you next time.
[music]