
A client had brain surgery and now has severe and painful spasms in their back. Is this a complication of surgery? Is this a precursor to total paralysis? Will massage make it worse? Listen for a brisk review of nervous system function and what happens when parts of the nervous system are injured. Upper or lower motor neurons—it makes a difference!
Resources:
Bell, Kathleen and Craig DiTommaso. “Spasticity and Traumatic Brain Injury.” Archives of Physical Medicine and Rehabilitation 97 (2016): 179–180. https://doi.org/10.1016/j.apmr.2015.05.010.
National Brain Tumor Society. “After Brain Tumor Treatment: Consequences of Treatment.” Accessed June 4, 2021. https://braintumor.org/brain-tumor-information/consequences.
Stanford Medicine. “Spasticity Versus Rigidity (25 Skills Symposium, 2015).” April 5, 2016. https://stanfordmedicine25.stanford.edu/blog/archive/2016/Spasticity-versus-Rigidity-Stanford-25-Skills-Symposium-2015.html.
Watanabe, Laurie. “Spasticity & Seating.” February 1, 2018. https://mobilitymgmt.com/articles/2018/02/01/spasticity.aspx.
https://commons.wikimedia.org/wiki/File:1615_Locations_Spinal_Fiber_Tracts.jpg
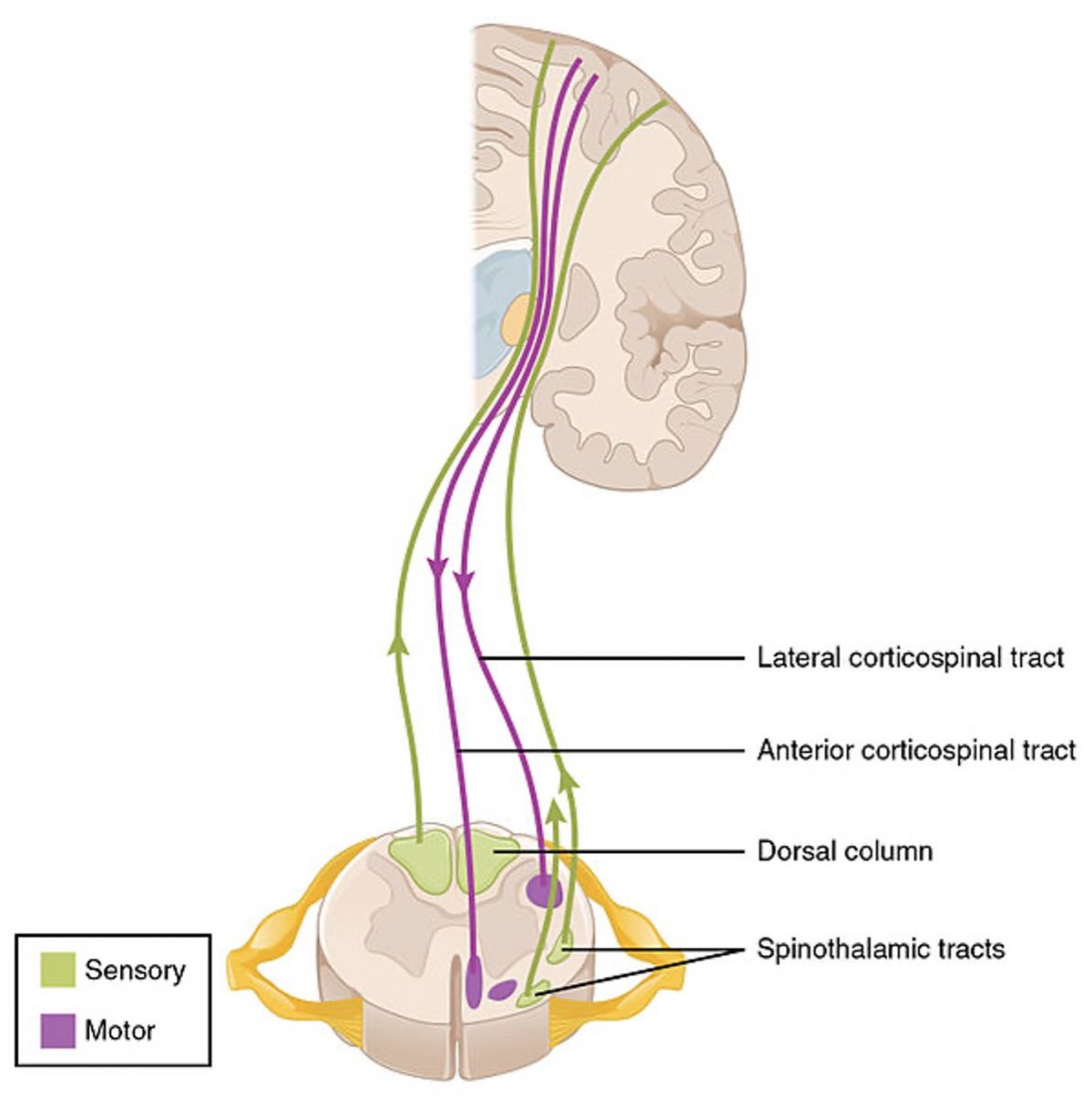
Cross section of spinal cord: note that the anterior horns are wider than the posterior horns. This is because the exiting motor neurons have their dendrites and cell bodies within the anterior horns. Descending motor tracts are in purple. Ascending sensory tracts are in green.


This podcast sponsored by:
About Anatomy Trains:
Anatomy Trains is a global leader in online anatomy education and also provides in-classroom certification programs forstructuralintegration in the US, Canada, Australia, Europe, Japan, and China, as well as fresh-tissue cadaverdissectionlabs and weekend courses. The work of Anatomy Trains originated with founder Tom Myers, who mapped the human body into 13 myofascial meridians in his original book, currently in itsfourthedition and translated into 12 languages. The principles of Anatomy Trains are used by osteopaths,physicaltherapists,bodyworkers,massagetherapists,personaltrainers,yoga,Pilates,Gyrotonics,and other body-minded manual therapists and movement professionals. Anatomy Trains inspires these practitioners to work with holistic anatomy in treating system-wide patterns to provide improved client outcomes in terms of structure and function.
Website:anatomytrains.com
Email:info@anatomytrains.com
Facebook:facebook.com/AnatomyTrains
Instagram: instagram.com/anatomytrainsofficial
0:00:00.0 Speaker 1: Ruth Werner's best-selling book, A Massage Therapist's Guide to Pathology, is a highly regarded comprehensive resource that sets the standard for pathology education. Written for massage therapy students and practitioners, this groundbreaking resource serves up a comprehensive review of the pathophysiology, signs, symptoms, and treatment of more than 500 diseases and disorders. Learn more at booksofdiscovery.com.
0:00:32.5 Speaker 2: Anatomy trains is happy to announce our return to the dissection lab in person, January 10th to the 14th, 2022 at the Laboratory of Anatomical Enlightenment in Boulder, Colorado. We are thrilled to be back in the lab with Anatomy Trains author Tom Myers and master dissector Todd Garcia. Join students from around the world and from all types of manual movement and fitness professions to explore the real human form, not the images you get from books. This is an exclusive invitation. Email info@anatomytrains.com if you'd like to join us in the lab.
[music]
0:01:17.1 Ruth Werner: Hi and welcome to I Have A Client Who... Pathology conversations with Ruth Werner, the podcast where I will discuss your real life stories about clients with conditions that are perplexing or confusing. I'm Ruth Werner, author of A Massage Therapist's Guide to Pathology, and I have spent decades studying, writing about and teaching about where massage therapy intersects with diseases and conditions that might limit our client's health. We almost always have something good to offer, even with our most challenged clients, but we need to figure out a way to do that safely, effectively, and within our scope of practice, and sometimes, as we have all learned, that is harder than it looks.
0:02:03.5 RW: Today's story comes from a Facebook post from a massage therapist in California who shares this very succinct question. Contraindications and suggested treatments/techniques for clients who have had brain tumour surgery in the past and have spasms as a result. Well, this gives me the opportunity to go down one of my very favorite rabbit holes, which is central nervous system injuries. I was able to get in touch with his massage therapist who gave me permission to share this story, and I learned a little bit more about this client. This is a new client, although they probably have had massage in the past. They are the partner of a good friend of the therapists, so everybody already knows each other. The client is in their late 40s and had brain surgery to remove as much of a tumour as was possible. And this was conducted about a year ago.
0:02:58.2 RW: Now this client is experiencing severe and extremely painful muscle spasms in their back. They've had back spasms in the past, but never this severe or painful. This massage therapist was concerned that something about this client's spine was affected either by the cancer or by the surgery and so was nervous about the safety of massage therapy. I'm so grateful for this person and the care and caution that they are taking about dealing with this client. Because this situation looks like it has a lot of ways things could go wrong if we don't know some of the ins and outs about central nervous system injuries. I'm not a neurologist, and I am no expert about central nervous system injuries and the way they are reflected in muscle tone. And the more I learn about this topic, the less I feel like I know, but I know a little bit. And this whole subject is incredibly intriguing.
0:03:57.9 RW: If I were ever to get back into practice, I would look for a setting where I could explore what massage therapy could do for clients who have had central nervous system injuries, traumatic brain injuries, stroke, spinal cord injuries. And that's what surgery is, of course, isn't it? It's scheduled trauma. So when I went to gather some information to share with you in this episode, I looked for what I could find out about spasm as a consequence of brain surgery. I couldn't find anything. But when I looked at spasm as a consequence of traumatic brain injury, tada, there was a lot. In order to talk about this, I want to do just a brief review of some of the functional divisions of the central and peripheral nervous systems. It's a topic that doesn't outline well but there are a few basic ideas to lay out here that will help us understand a little bit more about the safety of massage therapy for the client in this story.
0:04:57.4 RW: First of all, we will recall that the brain and spinal cord comprise the central nervous system, and the cranial nerves and the spinal nerves comprise the peripheral nervous system. And we know that those nerves that we talk about are bundles of fibers, and those fibers carry messages to and from and in between the central nervous system and the peripheral nervous system. We know that sensory neurons, those individual nerve cells that make up the bundles of fibers, sensory neurons carry messages from the body toward the spinal cord, and from the spinal cord up toward the brain. In the spinal cord, those neurons are bundled into tracks that carry messages upward. And the brain then assigns meaning to those incoming sensations. We also know that motor neurons carry messages from the central nervous system out into the body, where they interact, then, with muscles or glands at the direction of the spinal cord and the brain. I find it fascinating to realize that at our most mechanistic level, the sum of human response to stimulus is that we either contract something or we secrete something, or maybe both.
0:06:14.2 RW: And of course, there are those neurons that crossover in the spinal cord and throughout the brain, and their job is to link up that incoming sensation with outgoing motor responses, and these interneurons and brain cells, they give us the capacity to have reflexes, but also to think and remember things and learn things and have emotional reactions to things and so on. And that's all amazing, but it's not the topic that we're interested in today. So these central nervous system motor neurons, the ones that are carrying messages from the brain and down the descending tracks of the spinal cord, these ones are called the upper motor neurons. And then these descending tract neurons, they have a synapse with the outgoing motor neurons that run from the spinal cord out to those muscles and glands. And those motor neurons that are mostly in the peripheral nervous system, those are called lower motor neurons. And they have their tiny little dendrite and cell body within the spinal cord. And then they have these long, long axons that take those electrochemical messages out to their final destination.
0:07:23.3 RW: So that's a quick review of the motor and sensory construction of the nervous system, especially the peripheral nervous system. When someone has nerve damage, we often think of it as affecting sensation, or motor control, or maybe both. Sometimes there's another component that gets involved in this picture as well, and that's autonomic function. When someone has damaged to structures that are part of the autonomic nervous system, which is mostly motor, we expect to see problems then with digestion and regulation of heart rate and blood pressure and respiratory rate and sweating and other factors that are not related to skeletal or voluntary muscle. So all of this was to help brush off your mental picture of the functional relationships in the nervous system so that we can talk about the difference between upper motor neurons and lower motor neurons.
0:08:20.9 S1: Lower motor neurons, as we've said, have their dendrites and cell bodies in the anterior horn of the spinal cord. If you can imagine a cross section of the spinal cord in your head right now, you will remember that they're sort of an H-shaped extension of gray matter. And the posterior extensions of that H where the sensation enters the spinal cord, those are kind of thin, but the anterior extensions of the H are fatter, and they look that way because they're full of the dendrites and cell bodies of outgoing motor neurons, which exit the spinal cord on the anterior side. And I'll include a picture of this relationship in the show notes, in case you want to just refresh your memory about this. When something happens that damages lower motor neurons, the effect in skeletal muscle is almost always hypotonicity. When skeletal muscles lose their nerve supply, because the lower motor neuron has been impaired, those muscles tend to go very, very weak.
0:09:23.1 RW: By contrast, when something occurs that damages upper motor neurons, the ones that start in the brain or the ones that are held in the descending tracts of the spinal cord, the effect in skeletal muscle is much more likely to be hypertonicity and a situation that has the technical term called spasticity. The skeletal muscles tend to get very tight, they get hyperreactive, and if the damage is extensive and long lasting, we can see the skeletal muscles become contractures. That's a situation where the muscle is so constantly contracted, that it becomes a permanent state, and all of the connective tissue, fascial wrappings within and around that muscle, they shrink to fit. And it becomes difficult, if not impossible, to reverse this process.
0:10:12.4 RW: For reasons that I have never fully understood, when skeletal muscle becomes extra tight or develop spasticity because of that upper motor neuron damage in the battle between flexors and extensors, flexors almost always win. There can be hypertonicity on both sides of a joint, but eventually, as those muscles get tighter and tighter and tighter and tighter, the extensor muscles give up. And so, that joint, whether its fingers, or wrists, or elbows, or knees, tends to enter a state of flexion that becomes essentially permanent. Neurologists call this the clasp knife effect. And this is why when we look at the hands and arms and legs of people who have had an upper spinal cord injury, for example, we will tend to see that they are in a curled up position.
0:11:06.4 RW: Some central nervous system disorders, specifically Parkinson's disease, but it can occur with other things as well, result in a slightly different type of hypertonicity called rigidity of skeletal muscle, not spasticity. It's not technically the same. But the specifics of those differences are a topic for another day. If you're interested, I found a really nice educational piece comparing rigidity to spasticity that I will include in our show notes, because who knows, maybe this stuff intrigues you as much as it does me. But here's the deal. Those effects on skeletal muscles with upper motor neuron damage and spasticity, such as might have occurred with brain surgery that we see in his client story, those effects are almost always associated with the extremities, not with the trunk. Do you see why this matters?
0:12:05.6 RW: If this client were having signs of spasm and spasticity in her hands, or her feet, or her arms, or her legs, I would be concerned about upper motor neuron issues. That's not to say that massage therapy can't be helpful in these situations. In fact, my sense is that the role of massage therapy for people with these kinds of injuries is unexplored territory and we can probably do a lot more good than anyone who is exploring at this time. But in terms of having to worry about whether this client's muscle spasms are likely to become permanent or debilitating, because we're talking about postural muscles, and not muscles of the arms or legs, this seems probably unlikely. And I wanna say that this client's history has probably contributed to her spasms. People who have had traumatic brain injury or brain surgery tend to be hyperreactive to lots of different kinds of stimuli. And when I mentioned this to our contributor, they responded "Oh, yes, I know from their partner that there are some kinds of sounds that they just can't stand like the sound of metal cutlery." So they are familiar with this idea of hypersensitivity to certain kinds of stimuli.
0:13:15.1 RW: So my guess is that this person who's had brain surgery has some super reactive postural muscles. And something like stretching too fast or moving in an unexpected way, or some other kind of stimulus that we might never recognize, might have triggered this big muscular reaction. But that's different from the spasticity that we see with other kinds of central nervous system injury, and the role of massage therapy is much clearer. I advised this massage therapist to get a clear picture about the client's history because it's possible that they might have a shunt that needs to be accommodated for, and the chances are excellent that they are probably using some kind of pain medication or anti-seizure drugs to address nerve conduction. These drugs can be really effective, but they can also make people feel fatigued and low energy and we don't wanna make that worse with massage.
0:14:07.5 RW: Will massage therapy make this client's spasms go away? Yeah, it's hard to predict. I believe that massage therapy is gonna be safe and welcome for this client. I suggest that the therapist proceed with caution and see if they can identify what kinds of movements or pressures or stimuli are likely to trigger a spasm. But my guess is that these spasms are coming about because the person's nervous system is hyperreactive, and possibly with time and massage, and other relaxation techniques, maybe this person's nervous system can adapt and become more relaxed. And it's fair to say that massage therapy might be a significant contributor to that benefit. So I'm really happy that this person has found a massage therapist who is so interested to be safe and effective.
0:15:00.7 RW: Hey everybody, thanks for listening to I Have A Client Who... Pathology Conversations with Ruth Werner. Remember you can send me your I Have a Client Who stories to ihaveaclientwho@abmp.com. That's ihaveaclientwho, all one word, all lowercase, @abmp.com. I can't wait to see what you send me, and I'll see you next time.