Superior Outcomes
A treatment plan is what elevates massage therapy from a service to a therapeutic profession. It is the tangible output of our clinical reasoning.
Lateral knee pain is a common client complaint and is usually attributed to conditions such as iliotibial band friction syndrome, lateral meniscus lesions, and patellofemoral syndrome (runner's knee). However, an often-overlooked source of knee pain is hypomobility or instability at the proximal tibiofibular (tib-fib) joint (Image 1).
In this article, I'll describe the biomechanics and injury mechanisms of the tib-fib joint and then present a case study of a client with chronic knee pain that originated from an awkward judo fall.
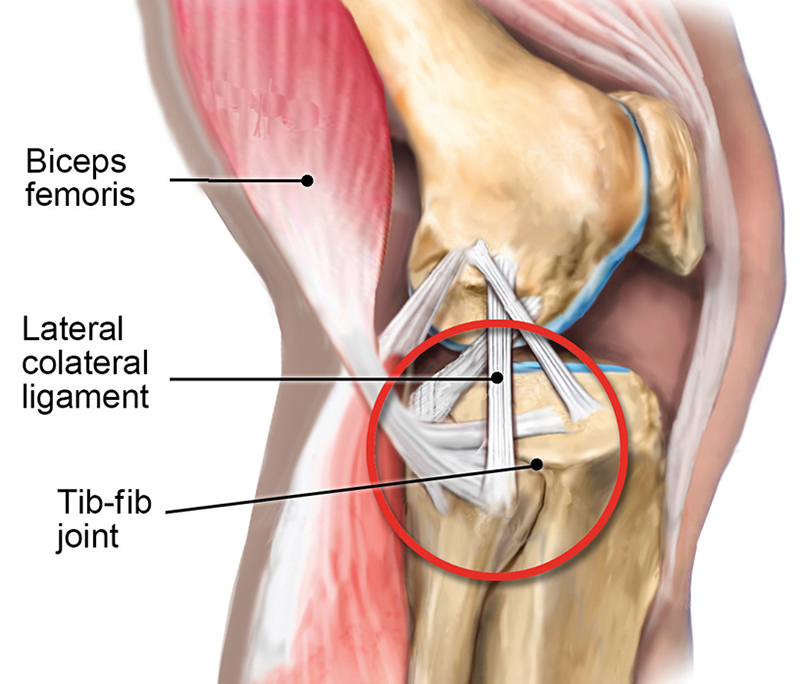
One of the primary functions of the tib-fib synovial joint is to help dissipate lower leg torsional stresses during gait. When the knee is extended, the biceps femoris, popliteus, and lateral collateral ligaments provide good joint stability. But with the knee flexed, these connective tissues lose much of their supportive capability. That's one reason tib-fib injuries are most often seen in sports that involve twisting forces around the knee and ankle, such as football, wrestling, soccer, judo, gymnastics, long jumping, and skiing.
In my nonathletic clients, tib-fib problems typically arise from overuse injuries on jobs that require repetitive activities. Clinically, I've found many clients presenting with lateral tib-fib pain from overuse also have an underlying body structure deficit, such as overpronated feet and valgus knees. In these cases, forces accumulate that cannot be properly dissipated or, worse, may be misdirected into areas not intended to handle the load, as we will see in the case study presented later in this article.
Common signs and symptoms of tib-fib dysfunction include:

Yale University researcher John Ogden, MD, was the first to conduct studies evaluating the anteroposterior (A-P) motion of the proximal fibula and correlating it with positional changes of the knee.1 He found that when the knee flexes, the proximal fibular head moves anteriorly, and during knee extension, the fibula translates posteriorly (approximately one centimeter in both directions). In Image 2, I demonstrate an assessment version of Ogden's A-P glide on my client Keith's right knee.
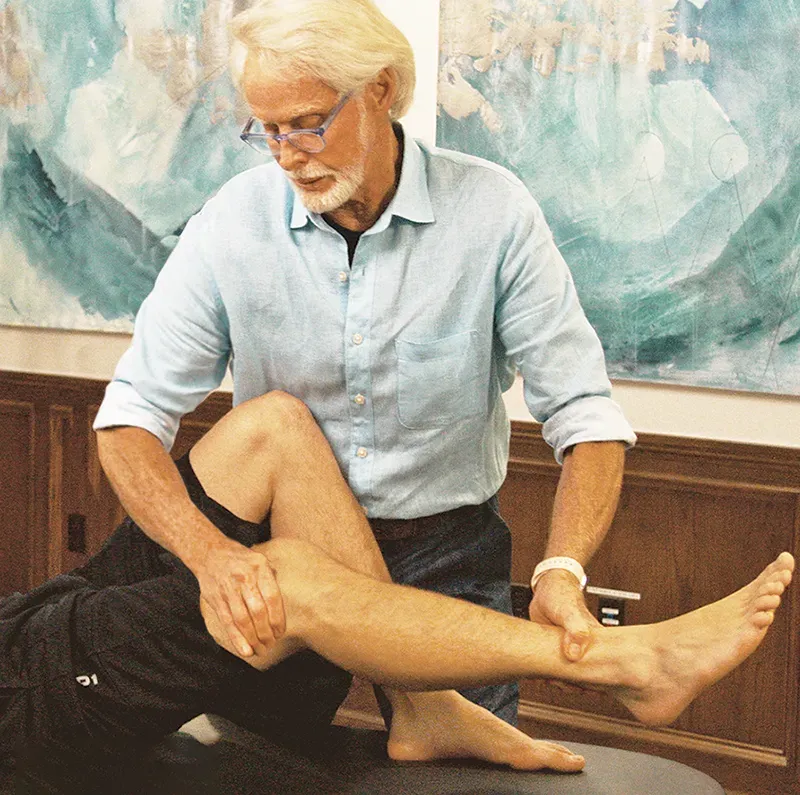
With index finger and thumb, I first locate a medium-size bump on his lateral leg about 2 inches inferior to the knee. To confirm I'm palpating the proximal fibular head, I simply flex Keith's knee to 90 degrees, locate the biceps femoris hamstring tendon just behind the lateral knee, and apply resistance as he attempts knee flexion (Image 3). If I feel the biceps femoris tendon tighten, I know I'm in the right spot.
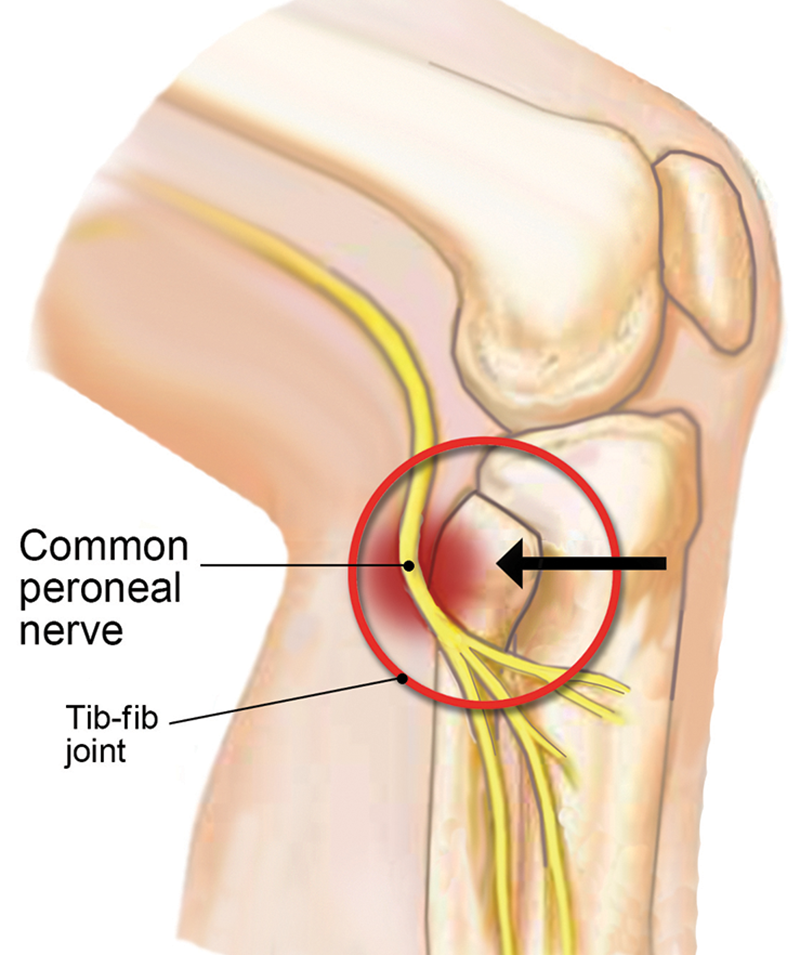
When assessing Keith's A-P glide, I noticed a restriction to anterior translation of the fibula on tibia accompanied by tenderness and a slight grinding noise. I recalled that during Keith's history intake he described a pretty significant inversion ankle sprain and hamstring contusion experienced during a judo fall that left him with a temporary limp, intermittent lateral knee pain, and lower leg numbness.
Using a clinical reasoning approach, I intuited that his posteriorly fixated fibular head might have resulted from shortening of the biceps femoris muscle following his traumatic judo injury. Further, I reasoned that Keith's intermittent lower leg paresthesia might have been triggered by common peroneal nerve irritation due to his posteriorly fixated fibular head (Image 4). To validate my findings, I asked Keith to stand on the affected leg and bend his knee to 30 degrees. This maneuver did reproduce Keith's knee and leg symptoms and is a very good confirmation test for tib-fib joint dysfunction.
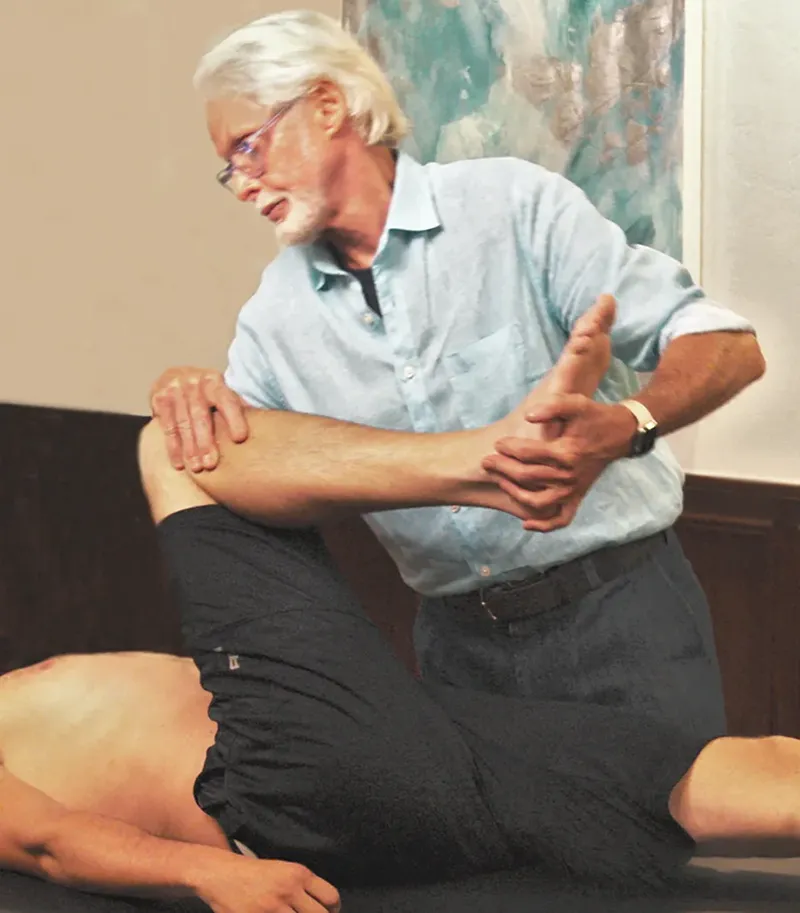
In Image 5, I apply a graded exposure hamstring stretching technique (using movement enhancers) to help relieve posterior drag of the biceps tendon from Keith's fibula. This stretching maneuver is great for those biceps femoris muscle injuries in which there is accumulated scar tissue and the brain is protectively guarding the area. Once I was able to improve Keith's hamstring flexibility, I chose a simple myoskeletal technique to help move the fibula forward on the tibia, then retested for improved tib-fib mobility (Image 6).

If you have a client with knee pain that fits some of the patterns outlined here, the tib-fib may be involved. In such cases, the first order of business is to determine the type and degree of tissue damage based on history, assessment, and clinical reasoning. Left untreated, tib-fib fixations can cause long-term difficulties, including pain, gait disturbance, and inferior sports performance. Hopefully, a better understanding of this often-neglected joint leads to less clinical error and improved client outcomes.
1. John A. Ogden, "Subluxation and Dislocation of the Proximal Tibiofibular Joint," Journal of Bone and Joint Surgery 56, no. 1 (January 1974): 145-54.
A treatment plan is what elevates massage therapy from a service to a therapeutic profession. It is the tangible output of our clinical reasoning.
Deep gluteal syndrome can be triggered by multiple causes. Sorting through those causes can be tricky, but doing so will also help your clients.
Context is powerful: Even light, mindful touch can significantly shift pain and proprioception, reminding us that how we work matters as much as what we do.
Considering the situation that led to your client’s pain can prove as valuable as understanding where the pain exists.