Featured Videos
-
Therapy Balls for pain relief and fascial reorganization.
-
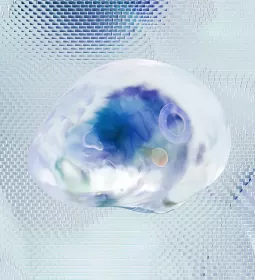
Examining the fibroblast cell and its functions in the body, including making up the fibers for the fabric of the human body.
-
Author Ruth Werner expands on her article about why people faint and interviews a first responder to dive deeper into the topic.
-
AnatomySCAPES debuts its video "The Sciatic Nerve: A 3D View from the Inside Out" in Massage & Bodywork magazine to dive deep into the sciatic nerve and its 3D fascial reality.